The $403 Million Lesson: How M&S’s Ransomware Attack Reveals the Critical Flaw in Modern Cybersecurity

You’ve probably invested thousands, maybe millions, in cybersecurity infrastructure—firewalls, encryption, monitoring systems. Yet despite all that technology, a single employee’s click just cost M&S $403 million in a devastating ransomware attack. This isn’t about outdated software or weak passwords. It’s about the one vulnerability your security budget can’t solve: human nature. The most sophisticated hackers […]
WheelHouse IT Secures SOC 2® Type 1 Certification—Joining the Elite Few MSPs That Put Their Security Controls to the Test

FOR IMMEDIATE RELEASE Fort Lauderdale, FL — February 27, 2025 — WheelHouse IT has successfully completed its System and Organization Controls (SOC 2) Type 1 examination, validating that the design of its security and availability controls meets the American Institute of Certified Public Accountants (AICPA) Trust Services Criteria as of February 27, 2025. The independent […]
Unleash Enterprise-Grade AI Security: How to Deploy GenAI Without Exposing Your Business to Catastrophic Risk
To deploy GenAI securely, you’ll need multi-layered defenses against five key risks: data poisoning, prompt injection, model extraction, privacy breaches, and supply chain vulnerabilities. Implement thorough data validation, input filtering, API rate limiting, and regular penetration testing. Watermark model outputs, establish contractual protections, and maintain regulatory compliance. With 68% of early adopters experiencing critical vulnerabilities, […]
Why Your MSP’s Security Posture Matters More Than Ever

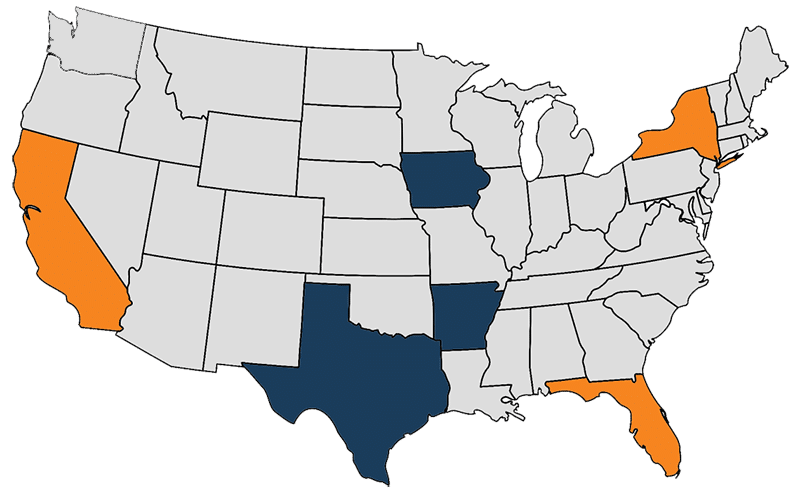
And how to tell if your provider is putting you at risk. In today’s threat landscape, working with a Managed Service Provider (MSP) is not just a convenience—it’s a liability if they’re not doing security right. Cyberattacks are no longer reserved for big-name enterprises. Small and midsized businesses are now prime targets, especially those in […]
Beware of Holiday Cyber Scams in 2024

As the 2024 holiday season approaches, the excitement of shopping and gift-giving is in the air. However, it’s also a prime time for cybercriminals who are eager to exploit the festive rush. Understanding the top holiday cyber scams can help protect yourself and your loved ones during this joyous yet vulnerable time. The Rise of […]