A Compliant EMR Doesn’t Make You HIPAA Compliant

Even if you’ve implemented a HIPAA-compliant Electronic Medical Records (EMR) system, it’s not enough to guarantee your practice’s overall HIPAA compliance. Complying with HIPAA involves more than just your EMR system – it extends to a broad range of areas, including administrative and physical safeguards, training, incident response, and regular updates to meet legal obligations […]
6 Reasons to Hire a HIPAA Compliance Consultant

It takes compliance experts with a deep understanding of the law to assess risks relating to a business, to properly train personnel, and to help compose policies and procedures regarding HIPAA compliance. That’s why we’ve compiled six reasons to hire one.
The Role of Technology in Advancing Healthcare

Technology revolutionizes your healthcare experience by improving disease diagnosis, treatment, and prevention. Tech advancements like AI, wearable devices, and mobile health apps optimize diagnostics, enhance patient care, and manage health more efficiently. Electronic health records offer secure, instant access to your medical information. AI analyzes complex data, detects subtle health changes, and aids in quality […]
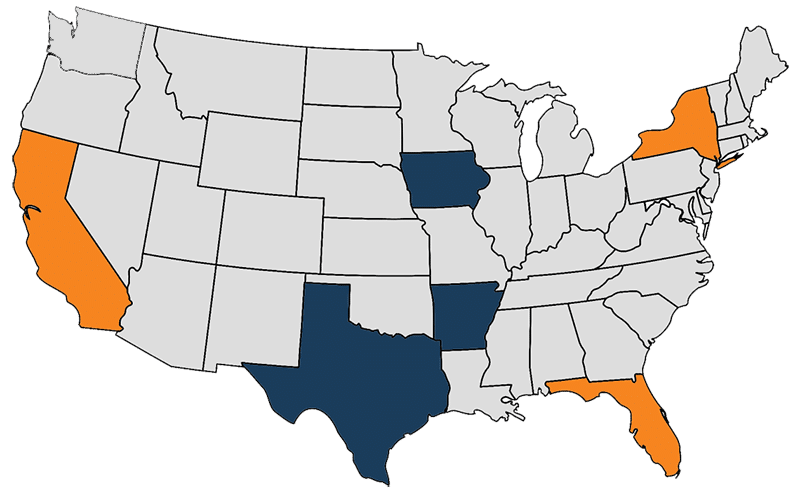
Navigating the Cyber Threat Landscape in Private Healthcare Practices: A Closer Look

The Challenge in Private Healthcare Practices In the increasingly digital world of private healthcare practices, the dual challenges of protecting sensitive patient information and ensuring uninterrupted care have never been more pronounced. With limited resources, reliance on legacy software systems, and the critical nature of the data they handle, private practices present an appealing target […]
Navigating HIPAA Compliance: Your Guide to Reporting Small Healthcare Data Breaches Before the Deadline

As we edge closer to the critical date of February 29, 2024, healthcare organizations are reminded of the looming deadline for reporting small healthcare data breaches, specifically those involving fewer than 500 records. This year, the calendar brings a slight twist with the leap year adjustment, setting the deadline a day earlier than the usual […]